Laparoscopic Cholecystectomy with Hernia Case 4
Conference Name: Laparoscopic Hernia Training Course
Surgeon(s)/Speaker(s): Dr. Ramesh Makam
Surgical Procedure: Laparoscopic Hernia-Umbilical hernia
Location: AV Hospital, Bengaluru
Indexsteps
1. OR Setup : * Patient lying supine with head up or down 15-20 degrees according to the type of hernia, for supra umbilical - head up and infra umbilical - head low *Surgeon stands on the left side, monitor on right side *S.R. Catheter and Ryle's tube are mandatory
2. Port Placement : * In all midline standard ventral hernias, the first port is very important. It may be a blind entry with a veress needle or an open entry but risk of injury to inner structures is high. Whether it is umbilical, epigastric or supra/infra umbilical incisional hernias with multiple scars, umbilical 1st port entry is impossible. Ports have to be placed away from all these defects, keeping in mind an overlap of 3-5 cm from all sides * Best 1st entry without any fear is left subcostal region i.e. Palmer point in the left mid clavicular line * After pneumoperitoneum is achieved, 1st entry with a 5 mm troacar through same point (Palmer point) is done. The 5 mm telescope with camera is passed for exact visualization of hernia defects, extent and nature of adhesions and size of hernia and probable size of the mesh * Two equidistant trocars, one 10 mm in the middle and 5 mm distal, are placed under vision. Once this is achieved, 10mm telescope with camera is passed through the middle port with two 5 mm trocars for working instruments * Note: For a big hernia defect supra umbilical, the first entry is further difficult. In such cases, an open entry technique is preferable
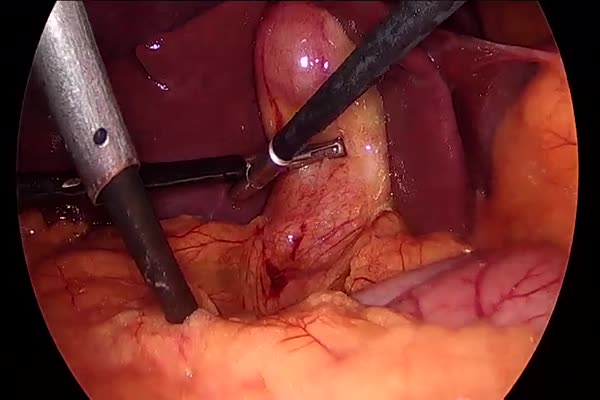
3. Adhesiolysis and reduction of sac contents : The following precautions need to be taken while doing this step * Utmost care while handling bowel, very slow and careful dissection * On site recognition of bowel injury * Minimal or no use of energy source (direct touch of hot tips) * Sharp dissection than blunt and pulling force which can produce serosal tears * In case of dense adhesions of bowel loops with peritoneum or old mesh, better to keep a part of the fascia/mesh with bowel * No inter bowel adhesions should be dissected unless you suspect acute kink or obstruction * If bowel is perforated / injured early recognition and repair is a must. If spillage of bowel contents or peritoneal soiling occurs, putting a mesh is debatable. Good peritoneal lavage must be done. Composite mesh is postponed or a biological mesh should be used * Once carefully all the adhesions are released (external pressure by assistant over the defect helps in adhesiolysis), sac is visualised for bleeding, control * Sac is not excised routinely but in some cases, part of big sac may be excised to avoid seroma * Incisions may be taken along the margin of the sac for better mesh adhesions to the wall * In supraumbilical hernia, round ligament / fat along the margins is excised for better placement of the mesh * Note: For suprapubic hernias a peritoneal flap is raised subpubically for the placement of distal part of mesh
4. Exact measurement of the defect or multiple swiss cheese defects : * Do not measure the defect with pneumoperitoneum as it may increase the size of the defect * Keep in mind shrinkage of mesh (upto 25%) * Best way is to cover all the defects with an overlap of 3-5 cms from all sides * Outline the defect in long and transverse axis using a spinal needle
5. Intraperitoneal onlay mesh (IPOM) : * Single mesh is used * In large defect, two pieces of mesh are needed, it weakens the repair * 4 sutures using 1-0 PDS or polypropylene (protine) are placed along long and transverse axis with knots on parietal surface, 1 cm inside the edge
6. Mesh introduction in peritoneal cavity : * Before introduction, the mesh is soaked in normal saline for 5-10 minutes in the same pack * Change of gloves * Mesh is rolled like a cigar with its visceral surface inside * Held with a grasper and introduced though a 10 mm port * Once inside, it is unrolled, spread with absorbable layer towards the bowel
7. Fixation of Mesh : * Transfascial sutures (you have put primarily or available with few meshes in the market) are pulled from outside using a port closure needle * Keep in mind * Equal overlap from all sides * No wrinkles on the mesh * Mesh must remain taught once the sutures are pulled * Small stab incision in the skin are made at the site of the inside sutures, both tails are pulled with a minimal distance to avoid pain and necrosis of the tissue between 2 tails * Absorbable or non-absorbable tacks are used to achieve additional fixation of the mesh * Tacks are put in 2 circumferential rows * 1st row of tacks is put 1 cm away from the edge of the defect at a distance of 2 cms from each other * 2nd row is put 2-3 cms away from 1st row, 5 mm away from the edge of the mesh * Apply pressure from outside over the abdominal wall making peritoneal surface perpendicular to tacker device * Confirm that there is no obvious defect left in the mesh and the peritoneal wall
8. Keen observation and closure : * See for any bleeding from adhesions / bowel * See for any spillage at the end of the surgery to diagnose inadvertent bowel injury * Tackle the injury properly, if any * 10 mm port is closed with port closure needle * The other 5 mm ports are also closed * Mini stab incisions are elevated to avoid puckering
9. Strapping abdominal wall : * Treatment of loose, redundant skin over the hernia defect * Pressure applied with a mop or gauze piece according to size * Tight elastocrepe pressure bandage applied for a minimum of 3 weeks * The above avoids seroma and skin gets adherent to posterior layers
port positions
1. Port placement : *In all midline standard ventral hernias, the first port is very important. It may be a blind entry with a veress needle or an open entry but risk of injury to inner structures is high.
*Whether it is umbilical, epigastric or supra/infra umbilical incisional hernias with multiple scars, umbilical 1st port entry is impossible. Ports have to be placed away from all these defects, keeping in mind an overlap of 3-5 cm from all sides.
*Best 1st entry without any fear is left subcostal region i.e. Palmer point in the left mid clavicular line.
precautionary_measures
1. Handling Bowel : Utmost care while handling bowel, very slow and careful dissection
2. Bowel Injury : On site recognition of bowel injury
3. Energy Source : Minimal or no use of energy source (direct touch of hot tips)
4. Sharp Dissection : Sharp dissection than blunt and pulling force which can produce scrotal (confirm) tears.
5. Adhesions of bowel loops : In case of dense adhesions of bowel loops with peritoneum or old mesh, better to keep a part of the fascia/mesh with bowel
6. Inter bowel adhesions : No inter bowel adhesions should be dissected unless you suspect acute kink or obstruction
7. Bowel perforation : If bowel is perforated / injured early recognition and repair is a must. If spillage of bowel contents or peritoneal soiling occurs, putting a mesh is debatable. Good peritoneal lavage must be done. Composite mesh is postponed or a biological mesh should be used.
8. Bleeding : Once carefully all the adhesions are released (external pressure by assistant over the defect helps in adhesiolysis), sac is visualised for bleeding, control
9. No sac is excised routinely : No sac is excised routinely
10. Part of big sac may be excised : In some cases, part of big sac may be excised to avoid seroma some people may take incisions along the margin of the sac for better mesh adhesions to the wall.
11. Supraumbilical hernia : In supraumbilical hernia, round ligament / fat along the margins is excised for better placement of the mesh
12. Suprapubic hernias : Note: For suprapubic hernias a peritoneal flap is raised subpubically for the placement of distal part of mesh
pre_post_measures
1. Preoperative investigations : Complete blood count:new: Blood sugar – random (fasting and postprandial, if diabetic):new: Serum creatinine:new: Liver function tests:new: Coagulation profile:new: HIV / HbsAg / Anti-HCV (if mandated by hospital):new: Blood group:new: Chest x-ray:new: ECG:new: Echocardiogram (if over 50 years):new: Abdominal ultrasound examination:new:
2. Preoperative measures : Patient is catheterized to empty the Bladder.:new: Attachment of the diathermy plate:new: Securing the patient to the table:new: Padding of the pressure points:new: Dose of prophylactic antibiotic at the time of induction of anaesthesia:new: Anti-embolic stockings / placement of an intermittent compression device on the legs:new:
3. Postoperative measures : NBM for 6 hours:new: Ambulate after that:new: Two dose of Antibiotics:new: Analgesics as required:new:
4. Warning signs in the postoperative period : Careful closure of the fascia at the umbilical trocar site:new: Infiltration of all trocar sites with local anesthetic:new: Closure of wounds and application of dressing:new: Pressure dressing is given on the Inguinal area to reduce Seroma.:new:
Surgical Instruments
1. 30 degree 10mm telescope
2. Veress needle
3. Suture
4. Bowel Grasper
5. Energy source
6. 10mm Trocar
7. Monopolar Electrosurgical Probe
8. Meril - Merinium Mesh
9. Epidural Needle
10. Maryland forceps
11. Meril - Profound A
12. L-Hook Monopolar Electrode
13. Atraumatic Graspers Plain
14. Monopolar Cautery
15. telescope
16. Maryland Dissector