Laparoscopic Nissens Fundoplication
Surgeon(s)/Speaker(s): Dr. Deepraj Bhandarkar
Surgical Procedure: Laparoscopic Gastrointestinal-GERD
Location: Sehaj Hospital, Indore
Indexsteps
1. Patient positioning : Patient is in a modified lithotomy position with head up by 25 degrees. Operating surgeon stands between patient’s legs, camera operator on patient’s right and second assistant on patient’s left
2. Inserting Laparoscope : Laparoscope is introduced through a port placed in the midline superior to the umbilicus.
3. Port placement : The 5mm trocars on either side allows for triangulation.
4. Liver retraction : Left lobe of the liver is retracted using a fan shaped retractor put through the anterior axillary port.
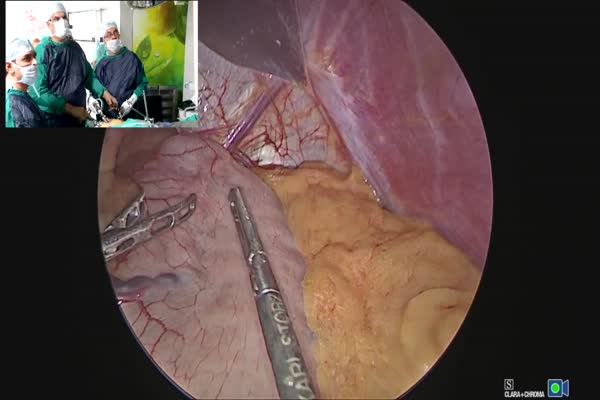
5. Dissection : Dissection started first by dividing short gastric vessels to mobilise the fundus using ultrasonic scissors
6. Left crus is mobilised : Left crus is mobilised taking care not to damage the phreno oesophageal ligament.
7. Gastro hepatic ligament is divided : Dividing the gastro hepatic ligament exposes the right crus:New:The right crus is then mobilised by dividing the peritoneum overlying the anterior aspect
8. Entering mediastinum : Enter mediastinum by blunt dissection along the medial side of the right crus
9. Visualise the esophagus : Visualise the esophagus
10. Circumferential mobilisation of esophagus : One the esophagus is visualised along with the crural confluence gentle blunt dissection avoiding injury to posterior vagus. Care is taken to not open the pleura.
11. Umbilical tape is put around the oesophagus : This helps to sling the oesophagus and also helps in retraction. Approximately 5-7 cms of intra abdominal oesophagus should be achieved after this
12. Crural closure is done : This is important to prevent the wrap from herniating into the mediastinum. This is achieved by placing a figure of 8 ethibond suture 2-0 gently approximating the crura:New: Excessive tightening of the crura may lead to dysphagia
13. Fundal wrap is constructed : 360 degree short floppy fundal wrap is constructed after placing a 50 fr bougie through the oesophagus into the stomach. The oesophagus should be enveloped by an untwisted fundus before suturing
14. Ensure Floppiness of the wrap : By shoe shine test and drop test
15. Wrap fixed using 2-0 ethibond sutures : The wrap should be 2-3 cms in length just above the OG junction. Adequate mobilization ensures 2-3 cms length of intra abdominal oesophagus above the wrap
16. Fundoplication suture line should face anteriorly : Fundoplication suture line should face anteriorly
17. Riles tube is left in situ and bougie is withdrawn : Riles tube is left in situ and bougie is withdrawn
18. Haemostasis ensured and ports closed : Haemostasis ensured and ports closed
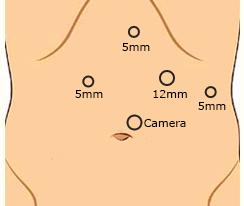
port positions
1. Port placement : * One 10 mm and three 5 mm trocars required
* Patient is in a modified lithotomy position with head up by 25 degrees. Operating surgeon stands between patient's legs, camera operator on patient's right and second assistant on patient's left
* Laparoscope is introduced through a port placed in the midline superior to the umbilicus.
* The 5mm trocars on either side allows for triangulation.
precautionary_measures
1. Phreno oesophageal ligament : Take care not to damage the phreno oesophageal ligament while mobilising the left crus
2. Left hepatic artery : *Take care not to damage the left hepatic artery while dividing the gastro hepatic ligament *During crural closure, Excessive tightening of the crura may lead to dysphagia
pre_post_measures
1. Preoperative investigations : CBC:new:Chest X-ray:new:EGD / endoscopy : to exclude stricture, Barrett’s esophagus, dysplasia and carcinoma:new:Barium Esophagogram : to define a non-reducible hiatal hernia, shortened esophagus:new: Esophageal Manometry: combined with impedance will identify ineffective esophageal peristalsis, misdiagnosed achalasia or scleroderma:new: ph testing : important for patients with non-erosive GERD or when uncertainty after EGD exists or for patients with esophagitis not responding to PPI.
2. Preoperative measures : Fasting for atleast 8 hours:new:Patient empties the bladder before coming to the theatre:new:Placement of a nasogastric tube:new:Attachment of the diathermy plate:new:Securing the patient to the table:new:Padding of the pressure points:new:Dose of prophylactic antibiotic at the time of induction of anaesthesia:new:Anti-embolic stockings / placement of an intermittent compression device on the legs
3. Postoperative measures : Monitoring of temperature, pulse and blood pressure:new:Allow the patient liquids after 4 – 6 hours and diet after 8 – 12 hours
4. Warning signs in the postoperative period : Nausea:new:Bloating, belching:new:Dysphagia:new:Bleeding:new:Excessive abdominal pain not related to flatulence
Surgical Instruments
1. 10mm Trocar
2. 5 mm Trocar
3. Liver Retractor
4. Ultrasonic Scissors
5. Blunt Dissector
6. Umbilical Tape
7. Suture 2-0