Laparoscopic Cholecystectomy Tubal Ligation
Surgeon(s)/Speaker(s): Dr. Lakshmi Kona
Surgical Procedure: Laparoscopic Cholecystectomy-Abdomen - Gall Bladder
Location: Gleneagles Global Hospital Hyderabad
Indexsteps
1. Diagnostic laparoscopy : Diagnostic laparoscopy to exclude any trocar-related injury and un-anticipated pathology.
2. Superior retraction of the fundus : Superior retraction of the fundus via a ratcheted grasper passed through the lateral trocar.
3. Lateral and downward traction of the Hartmann’s pouch : Lateral and downward traction of the Hartmann’s pouch via a grasper passed through the medial trocar.
4. Omental adhesiolysis : Omental adhesiolysis.
5. Visual appreciation of three critical landmarks : * Junction of the Hartmann’s pouch with the cystic duct. * Cystic lymph node if identified through the overlying fibro-fatty tissue. * Common bile duct.
6. Peritoneal incision : Peritoneal incision at the junction of the Hartmann’s pouch with the cystic duct.
7. Posterior dissection : Posterior dissection to free the Hartmann’s pouch from the liver bed.
8. Incision and dissection : Incision and dissection of the anterior peritoneal fold staying lateral to the cystic lymph node.
9. Clearing : Clearing of the cystic artery and cystic duct of all fibro-fatty tissue.
10. Creation of windows : Creation of windows between a) the cystic duct and cystic artery and b) between the cystic artery and the inferior edge of the liver.
11. Freeing up of the lower 1/3 of the gallbladder : Freeing up of the lower 1/3 of the gallbladder from the liver bed to expose the cystic plate (THE ABOVE THREE CONSTITUTE THE “CRITICAL VIEW OF SAFETY”).
12. Clipping and division : Clipping and division of the cystic artery.
13. Clipping / ligation : Clipping / ligation of the cystic duct.
14. Freeing up of the gallbladder : Freeing up of the gallbladder from the liver bed.
15. Confirmation of haemostasis : Confirmation of haemostasis on the liver bed.
16. Saline lavage : Saline lavage.
17. Placement of a drain : Placement of a drain in selected cases via the lateral / medial 5mm trocar site.
18. Closure of the fascia : Closure of the fascia at the epigastric 10mm trocar site with a suture using a suture passer device.
19. Placement of the gallbladder : Placement of the gallbladder in a plastic bag and retrieval via the umbilical trocar site.
20. Careful closure of the fascia : Careful closure of the fascia at the umbilical trocar site.
21. Infiltration of all trocar sites : Infiltration of all trocar sites with local anaesthetic.
22. Closure of wounds : Closure of wounds and application of dressing.
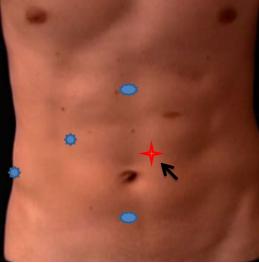
port positions
1. Port positions for Cholecystectomy : * Infra-umbilical 10mm trocar (camera port, inserted with closed technique using a Verres needle + sharp trocar or by open method)
* Epigastric 10mm trocar (placed around 2cm below the edge of the liver, just to the right of the falciform ligament)
* Lateral 5mm trocar (in the anterior axillary line, used for grasping and retracting the fundus superiorly)
* Medial 5mm trocar (in the mid-clavicular line, used for lateral and downward traction on the Hartmanns pouch. The position of this critical trocar varies depending on the size of the liver and location of the gallbladder)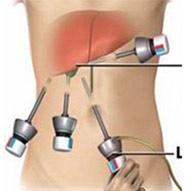
2. Port positions for Cholecystectomy : If needed 5 mm additional port for retraction on Left side of Umbilical port.
precautionary_measures
1. Precautionary Measures for this surgery : 1. For easy handling Drain GB if distended. 2. Use short bursts of energy source. 3. Keep a gauge inside helps for pressure in bleeding, good for blunt dissection. 4. Do not use Energy source near CBD. 5. Do not use CLIPS unless Critical view is clear. 6. Do not use unnecessary clips. 7. Choose right size of clip judge C duct diameter perfectly at times use ligature. 8. Collect every spilled out stone, good wash if Bile leaks.
pre_post_measures
1. Preoperative investigations : Complete blood count :new:Blood sugar – random (fasting and postprandial, if diabetic) :new:Serum creatinine :new:Liver function tests :new:Coagulation profile :new:HIV / HbsAg / Anti-HCV (if mandated by hospital) :new:Blood group :new:Chest x-ray :new:ECG :new:Echocardiogram (if over 60 years) :new:Abdominal ultrasound examination :new:MRCP / endosonography, if -Abnormal liver function tests (raised transaminases / alkaline phosphatase / ΥGT -Suspicion of bile duct stones (previous pancreatitis / obstructive jaundice)
2. Preoperative measures : Patient empties the bladder before coming to the theatre :new:Placement of a nasogastric tube :new:Attachment of the diathermy plate :new:Securing the patient to the table :new:Padding of the pressure points :new:Dose of prophylactic antibiotic at the time of induction of anaesthesia :new:Anti-embolic stockings / placement of an intermittent compression device on the legs
3. Postoperative measures : Monitoring of temperature, pulse and blood pressure :new:Allow the patient liquids after 4 – 6 hours and diet after 8 – 12 hours :new:Two more doses of antibiotics (unless an extended antibiotic therapy is required for acute cholecystitis) :new:Intravenous analgesics for the first 24 – 48 hours changed to oral analgesics at discharge :new:Anti-emetics for the first 24 hours :new:Intravenous fluids for the first 6 - 12 hours :new:Discharge once the patient is relatively pain-free, tolerating diet, ambulatory and WILLING TO GO HOME
4. Warning signs in the postoperative period : Patient feels unwell beyond the first postoperative day :new:Severe nausea / vomiting beyond first 24 hours :new:Tachycardia :new:Hypotension :new:Fever :new:Respiratory distress :new:Abdominal distension / marked tenderness / guarding / rebound tenderness / absent bowel sounds :new:Presence of bile in the drain
Surgical Instruments
1. 10mm Trocar
2. Reducer (10mm to 5 mm)
3. Fundus Grasper with Ratchet
4. Non-traumatic grasper
5. Maryland Dissector
6. Suction Irrigation canula
7. Clip applicator
8. Ultrasonic Shear
9. Port closure needle
10. Specimen retrieval bag
11. 5 mm Trocar
12. Laparoscopic Scissor
13. Electrosurgical Unit
14. Atraumatic Graspers Plain
15. L-Hook Monopolar Electrode
16. Monopolar Cautery
17. Curve Scissor Metzanbaum
18. Grasping Forceps Traumatic
19. Laparoscopic Polymer Clips
