Diverted Long pouch Gastric Bypass
Education event Sponsored by: FourZone
Conference Name: Advancements in Metabolic Surgery for Diabetes Management
Conducted by: Fourzone healthcare LLP & Dr. Parag Patel
Surgeon(s)/Speaker(s): Dr. Parag Patel
Surgical Procedure: Bariatric-Sleeve Gastrectomy
Location: GOBESITY, Zydus Hospital, Anand
Indexsteps
1. Position and Placement : The patient is supine on a dedicated bariatric surgical table with supports for the feet and straps to secure the patient as often the surgeon needs a rather steep head up position to get access to the upper stomach. intermittent pneumatic compression devices are in place along with a patient warming blanket. Two image monitors are placed at the level of the patient's shoulder on either side for uninterrupted viewing by the surgeon and his assistant. Once the anesthetic team have gained good vascular access with the monitoring devices in place the surgical team comes into position, the surgeon often stands on the right side of the patient with the assistant on the left side. The camera person standing the right of the surgeon and the scrub nurse is positioned next to the camera person or next to the assistant surgeon on the left side of the patient. It is always worthwhile to check the various energy settings, insufflator settings, the necessary devices, staplers and cartridges availability before starting the surgery. The surgeon has to have a constant dialogue with the anesthetist, assistant and the scrub nurse especially during positioning and changing the gastric calibration bougies, introduction and with drawl of long bariatric instruments and staplers so that technical errors and collateral damage is minimized.
2. Gastric decompression : A distended stomach (fluid and air) poses technical difficulties in grasping and handling the stomach. Hence good gastric decompression is needed to ensure a easy and safe dissection. The stomach can be decompressed either with an orogastric ryle's tube or by using the side channel of a gastric calibration bougie.
3. Mobilization of greater curvature : The greater omentum is taken down using energy device (harmonic shear, ultrasscion etc) starting at a point about 4cms-6 cms proximal to the pylorus. the dissection is carried out cephalad and the gastric fundus is mobilized in its entirety taking adequate care to safe guard the spleen especially when there are omental and ligamentous adhesions.
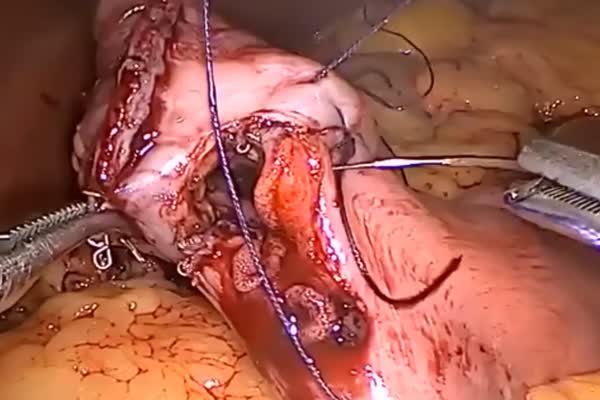
4. Creation of the gastric tube : A 32-36 Fr gastric bougie is placed by the anesthetist and is guided by the surgeon along the lesser curve until its down the pylorus. The gastric stapling device (endo GIA) is introduced and the stomach is stapled starting from the point about 4-6 cm from the pylorus. Sequential stapling is done in the cephalad direction until the entire stomach is divided. Care is taken to avoid injury to the pancreas and spleen; staple position and sleeve size is frequently checked to avoid a tight or lax sleeve and to avoid a spiraling staple line due to uneven incorporation of the anterior and posterior gastric walls.
5. Assessing staple line integrity : The bougie is gently withdrawn proximally and air insufflation is done so that the surgeon can check for air leaks by instilling saline over the stapling line. At times a persistent ooze is encountered at specific points along the staple line that needs to be addressed by applying a ligaclip rather than using energy sources as the staples conduct the energy into the deeper tissues. There also exists the practice of placing a layer of surgical wrapping the staple line or re-enforcing the staple line by applying a row of invaginating sutures or by using buttressing materials although this is not standard or mandatory practice.
6. Specimen extraction : The resection stomach is extracted via the umbilical port under vision with the camera being introduced via the 13 mm right sided port. All ports 10 mm and above are closed with vicryl sutures under vision with or without the aid of a port closure device.
7. Liver retraction : The liver is elevated and this provides adequate visualization of the entire stomach during the gastrectomy.
port positions
1. Port placement : A 10 Mm Umbilical Or Sub Umbilical Port Is Placed By Open Or Closed Technique As Per The Local Unit Practice Or Protocol. Five Millimeter Ports Are Placed In The Left Mid-Abdominal, Left And Right Upper Quadrants Along With A Sub Xiphoid Port For Retracting The Left Lobe Of The Liver. A 13 Mm Port Is Placed Is Placed Along The Right Mid Abdomen For Passage Of The Stapler Device.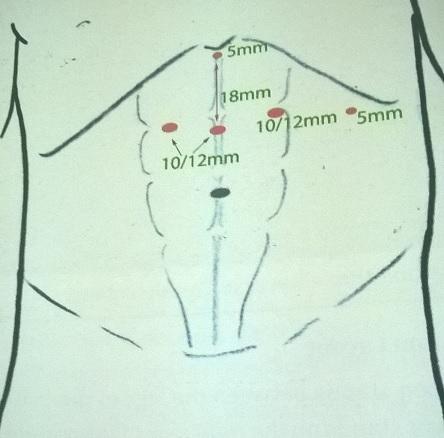
precautionary_measures
1. Dissection : During dissection, care should be taken to avoid injury to short gastric vessels
2. Large vessels : Surgical clips should be used for large vessels
3. Using a stapler : While using a stapler, care should be taken to avoid the esophagus from the staple line.
pre_post_measures
1. Preoperative investigations : The morbidly obese individual undergoing a bariatric surgical procedure presents a unique set of difficulties to the anesthetists, surgeons, nurses in the operating suite, recovery and the wards. Hence it needs a dedicated team to ensure safety and success in all aspects to run a successful bariatric program. A thorough pre-operative work-up and multi-disciplinary team assessment is the vital first step in the whole process. This includes :new: Detailed history and physical examination :new: Hematological investigations: complete blood count, blood group, coagulation profile :new: Biochemical investigations: liver function tests, kidney function tests, lipid profile, blood glucose (fasting and postprandial). :new: Micronutrient element levels: vitamin B12, Iron, ferritin, folic acid, vitamin D :new: Cardiac investigations: ECG, Echo, Stress test :new: Pulmonary investigations: CXR, Sleep study :new: Gastroenterology: OGD, USG for gallbladder status :new: Endocrine tests: HbA1c; thyroid-stimulating hormone.
2. Preoperative measures : Weight loss and exercise regimen: After the multi-disciplinary team evaluation, the patient is prescribed a tailor made dietary and exercise program. The dual benefits of this strategy is to ensure that patient homeostasis is optimized for the planned surgery and to asses actual patient compliance that is crucial to the long term surgical outcomes. A 5%-10% weight loss is a good indicator of patient compliance and is associated with a positive outcome. Patients are encouraged and supported in their endeavor to quit smoking ( at least 6-8 weeks prior to planned surgery) due to increased respiratory and cardiovascular adverse effects of the duo of risk factors (smoking and morbid obesity). Male pattern of fat distribution, especially in the upper abdomen, in the greater omentum and small bowel mesentery is an hindrance to bariatric surgery, as access to the proximal stomach and the esophago-gastric junction (OGJ) is restricted. The left lobe of the enlarged, fatty liver in many bariatric surgical candidates poses technical issues and an injury hazard during surgery as it obstructs the views and access to the proximal stomach and hiatal areas; manipulation of the liver risks bleeding, sub capsular hematoma and parenchymal fractures. A 4-6 week pre-operative low calorie diet reduces liver size and intra-hepatic fat that aids the bariatric surgeon to handle the liver safely and gain better exposure during bariatric procedures. :new:Multi-disciplinary team The morbidly obese patients are intricately complex patients who pose significant challenges to all the teams involved in the pre-operative care of a bariatric surgical patient. Hence its vital to have a team of well qualified and experienced specialists in their respective faculties. The trials and tribulations of a new bariatric unit in its endeavor to be a successful unit is a testimony to the complex physical and physiological aspects of a demanding morbidly obese surgical candidate. Regulations and resources regarding competency, infrastructure and support services go a long way in assuring the success of any bariatric program. The potentially enrolled surgical candidates who satisfy the selection criteria are then evaluated by the team of specialists that include :new:anesthesiologists :new:cardiologists :new:pulmonologists :new:endocrinologists :new:diabetologists :new:bariatric nurses :new:nutritional therapists :new:psychiatrists :new:physiotherapists :new:psychologists
3. Postoperative measures : Bariatric surgery follow-up measures Having undergone a bariatric surgical procedure, the patient and family should realize that surgery is just the initial step in the long journey to weight loss. In this phase, patient compliance, motivation and support from friends and family is vital for positive physical, psychological and social outcomes. Regular visits and contact with the surgical team, physiotherapists and nutritional experts are crucial to ensure that weight loss is sustained and nutritional and micronutrient deficiences are minimized. :new:The follow up protocols vary from unit to unit and from region to region. By and large, after the initial recovery, the hospital visits are scheduled 3 months post-operatively, subsequent visits are once in 6 months for three years and then annually for life. :new:The assessment protocol would include a consultation, history and physical examination with specific focus on micronutrient deficiences, endocrine function, skin tone quality and muscle mass. :new:Investigations would include a complete blood count, glucose level, lipid profile, Hb1Ac, Iron, ferritiin, vitamin-D, folate and vitamin B12 levels.
4. Warning signs in the postoperative period : The complications of sleeve gastrectomy include -hemorrhage -leak -intra-abdominal abscess -stricture -GERD :new:Staple line leak: One of the major complications of LSG is staple line leak. An early leak is one that is diagnosed usually by the third post operative day. In contrast leaks diagnosed after 8 days of surgery are termed a late or delayed leak. Any unexplained tachycardia during the postoperative period should raise the suspicion of a gastric staple line leak. Depending on the timing, extent of leak, presence of abdominal collection and patient status the leaks are managed by using the standard measures that include initial intravenous fluids and antibiotics, stopping all oral intake, placement of a stent, placement of a nasojejunal feeding tube, percutaneous drainage of abdominal collections, laparoscopy for washout, drainage of collection and placement of abdominal drains. :new:Among the late or chronic complications, stricture often presents with dysphagia, nausea and vomiting, the common site of stricturing is at the incisura and can be diagnosed by a gastrograffin study or upper gastrointestinal endoscopy. Chronic strictures can be dilated endoscopically, when endoscopic techniques fail especially when the stricture is long, surgical interventions is necessary. Performing a seromyotomy or converting to a roux-en-y gastric bypass is often needed.
Surgical Instruments
1. EndoZone Stapler
2. TriZone GC
3. Laparoscopy Hand Instrument
4. CO2 Insufflator
5. Stapler
6. Liver Retractor
7. 10mm Trocar
8. 5 mm Trocar
9. telescope
10. Maryland
11. Suture
12. Veress needle
13. Atraumatic Grasper
14. Scissors
15. Needle Holder Straight
16. Needlr Holder Curved
17. Needle Holder Curved
18. Monopolar Electrosurgical Probe
19. Fenestrated Double Slit Curve Grasping Forceps
20. Curve Scissor Metzanbaum
21. L-Hook Monopolar Electrode
22. Maryland Dissector
23. Maryland Dissector
24. Maryland Dissector Long
25. Suction